April 7, 2016 Print
One of Australia’s leading diabetes researchers has warned that the rapidly increasing incidence of type 2 diabetes and associated complications threatens to break the nation’s healthcare budget.
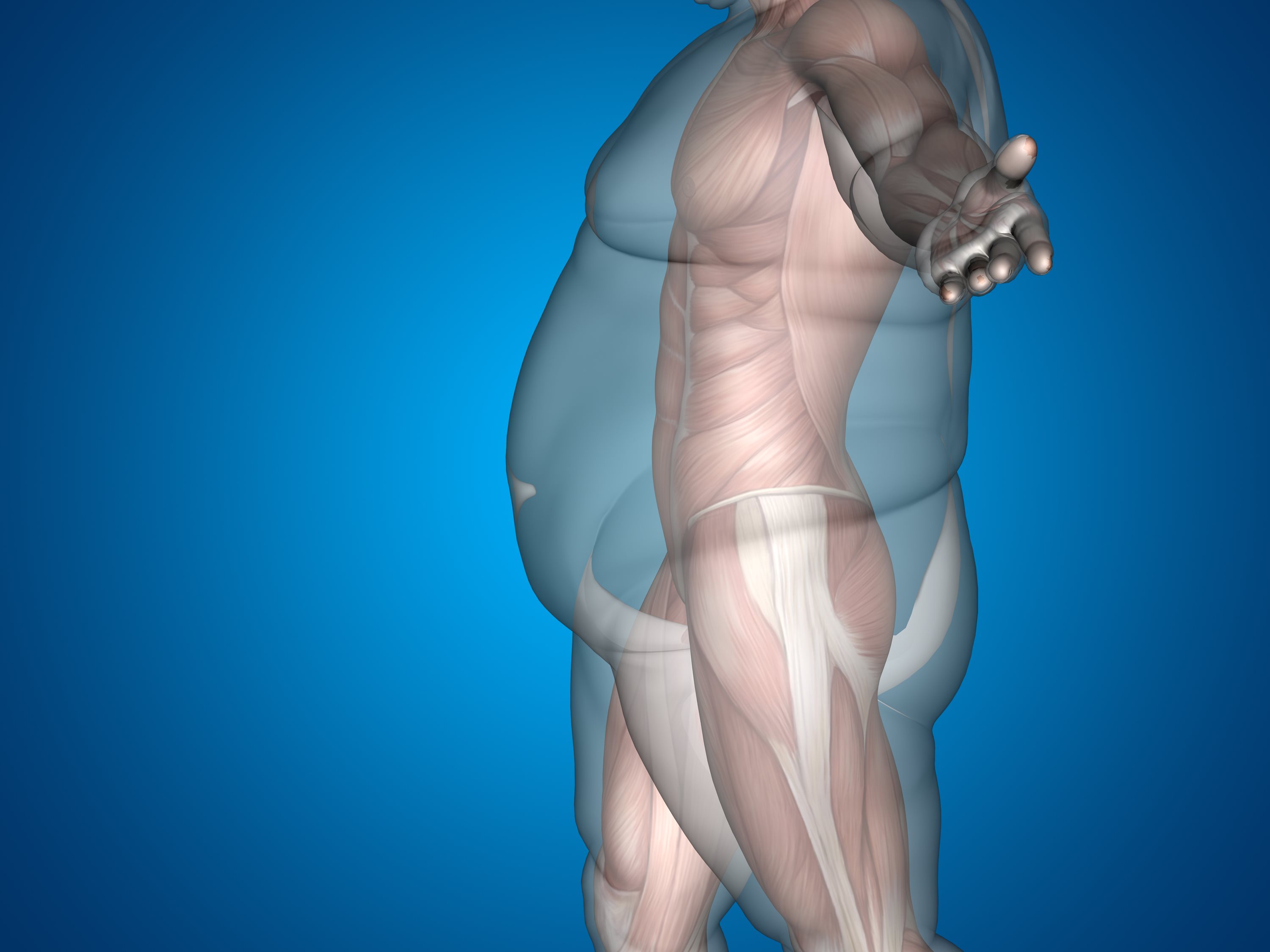 Type 2 diabetes is a multi-system disorder casued by obesity and inactiveity
Type 2 diabetes is a multi-system disorder casued by obesity and inactiveity
Speaking on World Health Day (April 7) – which has the theme ‘Beat Diabetes’ – the director of The Westmead Institute’s Centre for Diabetes, Obesity and Endocrinology, Professor Jenny Gunton said type 2 diabetes is a multi-system disorder which is causing big increases in the rate of kidney, liver and eye diseases.
“The knock-on effects of the explosion in diabetes are big increases in other chronic illnesses and a growing and unsustainable burden on the health system,” Professor Gunton said.
In an effort to address the looming problem, the Westmead Institute is forging trans-disciplinary partnerships between its different research groups to tackle the disease.
“At the Westmead Institute we have many different groups that bring together expertise to tackle this epidemic,” said Professor Gunton.
“Having a critical mass of expertise saves time and money and leads to innovative solutions.
“As a result, we now have an understanding of some of the factors which lead to kidney failure, and some of the liver problems of diabetes such as increasing fat, inflammation, and an increased risk of liver fibrosis.”
“As a result, we now have an understanding of some of the factors which lead to kidney failure, and some of the liver problems of diabetes such as increasing fat, inflammation, and an increased risk of liver fibrosis.”
Professor Gunton’s team is investigating ways to improve transcription factors – master regulators of the endocrine system – to encourage weight loss and improve type 2 diabetes control.
“The hope is that, by tweaking the activity of these factors, we can give optimal function to the cells to help control diabetes, fatty liver and obesity,” Professor Gunton said.
Groundbreaking work by Professor Jacob George and the Institute’s Storr Liver Centre identified insulin resistance as the universal underlying pathophysiological abnormality in fatty liver disease.
This now underpins the majority of research on this condition and is the cornerstone of current therapy, which includes lifestyle intervention such as exercise.
“Around 25 years ago we never saw fatty liver disease. Now, in the last 20 years, we’ve seen more and more patients presenting with end stage liver disease, liver cancer and liver failure,” Professor George said.
“When we looked at these patients in more detail, we realised that they were developing liver disease for the same reason they were developing diabetes: obesity and an inactive lifestyle.”
Professor Gunton says that thanks to collaborative research efforts, progress is being made in the fight against diabetes and associated diseases.
Professor Gunton says that thanks to collaborative research efforts, progress is being made in the fight against diabetes and associated diseases.
“Our treatments for diabetes have improved steadily over many years. The outcomes per person with diabetes are much better than they were 30 or 40 years ago. An individual with diabetes has a lower risk of blindness, kidney failure and amputation than in the past,” Professor Gunton said.
But while individual risk of some diabetes complications has decreased due to recent medical advances, Professor Gunton says the total number of people with diabetes is increasing at an alarming rate and more needs to be done to address this growing epidemic.
“We are aware of well over one million people in Australia who have diabetes now. That rate is increasing because of age, obesity and lack of exercise.”
Professor George says the obvious and simple fix is to lose weight and increase exercise, but that is much easier said than done. “Despite everyone agreeing that it is a good thing, in the last 20 years, Australians have become more inactive and their weight has increased,” he said.
The Westmead Institute: other diabetes-related research in focus
Kidney research
According to Professor David Harris, who heads the Institute’s Kidney Injury Repair and Fibrosis Study Group, the main cause of kidney failure worldwide now is diabetes.
“About one in ten Australians has signs of chronic kidney disease, and about 25, 000 patients in Australia have end stage kidney disease where they require dialysis or a kidney transplant to stay alive,” Professor Harris said.
“Our research is focused on fibrosis and inflammation within the kidney and the role that plays on the progression of kidney disease. More particularly, we are looking at developing novel therapies to prevent inflammation and fibrosis and slow the progression of disease.”
Professor Harris says their research is making significant advances in the treatment of fibrosis and also in the treatment of inflammation.
Vision research
At the Institute’s Centre for Vision Research, scientists are exploring if subtle alterations in the blood vessels around the eye can help predict diabetic eye disease.
Diabetic eye disease is one of the most frequent and devastating complications of diabetes and is the leading cause of blindness is adults aged 20-74.
At Westmead Hospital, Dr Gerald Liew and his team will be trialling new treatments for diabetic macular oedema, which is the main cause of vision impairment in diabetic eye disease.
According to Dr Liew, current standard treatments for diabetic macular oedema is limited to repeat injections of agents to the eye, or focal laser, which are costly, invasive, and carry significant risks including risks of blindness.
Islet transplantation for type 1 diabetes
At the other end of the spectrum, researchers from the Institute’s Centre for Transplant and Renal Research are giving hope to type 1 diabetes sufferers by refining a process that can negate the need for daily insulin injections.
Type 1 diabetes is an auto-immune disease which destroys the body’s insulin producing cells. About 10 per cent of sufferers are affected by hypoglycaemia unawareness, which causes the body’s blood sugar levels to fall without the person realising – a situation that could potentially trigger seizures, loss of consciousness, brain damage or even death.
Scientists at The Westmead Institute and Westmead Hospital established Australia’s first successful trial of a relatively non-invasive procedure in which insulin-producing pancreatic islet cells are taken from donor organs and transplanted into a recipient’s liver.
Scientists at The Westmead Institute and Westmead Hospital established Australia’s first successful trial of a relatively non-invasive procedure in which insulin-producing pancreatic islet cells are taken from donor organs and transplanted into a recipient’s liver.
Now, Associate Professor Wayne Hawthorne and his team are working to refine this process, and ultimately help more and younger sufferers.
“Currently, we lose about 60-80 per cent of the islets in the islet isolation process. This means that we have to transplant two or even three pancreases for a single recipient,” Associate Professor Hawthorne said.
“We are trying to expand on our ability to isolate islet cells and offer a broader number of transplants to more patients.
“As a result of our research, we are now extracting more islet cells more efficiently, which means that patients who didn't previously have any treatment options now have hope.”
“As a result of our research, we are now extracting more islet cells more efficiently, which means that patients who didn't previously have any treatment options now have hope.”