June 21, 2019 Print
New cells are more susceptible to HIV infection and transmit virus to other cells.
 Members of the research team. (Left to right) Heeva Baharlou, Associate Professor Andrew Harman, Kirstie Bertram.
Members of the research team. (Left to right) Heeva Baharlou, Associate Professor Andrew Harman, Kirstie Bertram.
Researchers at The Westmead Institute for Medical Research have discovered brand new immune cells that are at the frontline of HIV infection. Known as CD11c+ dendritic cells, these new cells are more susceptible to HIV infection and can then transmit the virus to other cells.
CD11c+ dendritic cells are a subset of dendritic cells (a type of immune cell) that are only found in human genital tissues, specifically at the epithelial level (the thin layer of tissue that forms the surface) of the vagina, inner foreskin and anus. This location in genital tissue often means that these newly discovered CD11c+ dendritic cells are the first immune cells to interact with HIV.
One of the lead researchers on this project,
Associate Professor Andrew Harman from The Westmead Institute for Medical Research says that the role of these newly discovered CD11c+ dendritic cells is to capture any incoming disease-causing virus or bacteria (pathogen), and then deliver it to CD4 T cells.
“CD4 T cells are responsible for driving an immune response to the pathogen. Interestingly, they are also the primary HIV target cells in which the virus replicates.
“Once dendritic cells capture a pathogen, they communicate what they have found to CD4 T cells in the
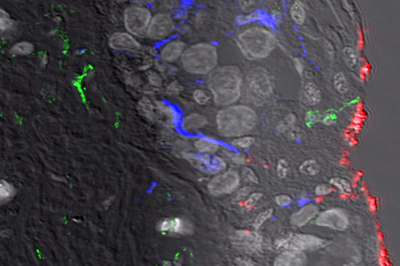 The image shows sampling of HIV (red) by the newly described epidermal dendritic cell (green).
The image shows sampling of HIV (red) by the newly described epidermal dendritic cell (green).
lymph nodes, essentially giving the immune system a constant update. This information prepares the immune system to either tolerate a bacteria or virus, or attack it.
“However, if CD4 T cells fall below critical levels (e.g. in HIV positive patients), then the body is no longer able to mount an immune response, leading to a diagnosis of AIDS.
“Our research team has shown that the newly discovered CD11c+ dendritic cells are more susceptible to HIV infection than any other known dendritic cell. We have also shown that CD11c+ dendritic cells interact with CD4 T cells more efficiently than any other dendritic cells. Importantly CD11c+ dendritic cells transfer the virus to CD4 T cells, making them key drivers of HIV infection. As these dendritic cells are so efficient at interacting with CD4 T cells, they are also important vaccine candidates.
The team from The Westmead Institute for Medical Research were able to discover these CD11c+ dendritic cells using donated genital tissues. Associate Professor Harman says, “We were able to look at the tissue only 30 minutes after it had been surgically removed from the body and also developed ground breaking RNAscope technology which allowed us to watch as living CD11+c dendritic cells took up the virus and delivered it to the CD4 T cells,” says Associate Professor Harman.
 Professor Tony Cunningham
Professor Tony Cunningham
According to co-lead author and Executive Director of The Westmead Institute for Medical Research,
Professor Tony Cunningham, this discovery has unlocked two new avenues for medical researchers to pursue in the search for more effective HIV treatments.
“This finding opens up a potential for the development of strategies to block the transmission of HIV. If we can block HIV’s ability to bind to the CD11+c dendritic cells, which are often the first immune cells to encounter the HIV virus, then we can stop their ability to transmit the virus to the CD4T cells. In a situation where there are low levels of CD4 T cells, this could stop the virus from spreading.
“Another avenue is to use this new information to develop a HIV vaccine. If HIV fragments or inactivated HIV were targeted at these CD11+c dendritic cells, this would have the potential to prime an immune response against HIV as soon as it enters the body,” says Professor Cunningham.
This research finding is published in
Nature Communications.
The research was supported by funding from the National Health and Medical Research Council (NHMRC).
Associate Professor Andrew Harman is affiliated with The Westmead Institute for Medical Research and The University of Sydney School of Medicine.
The study was carried out with the assistance of:
- Centre for Virus Research, The Westmead Institute for Medical Research
- The University of Sydney
- Institute of Cellular Medicine, Newcastle University, Newcastle upon Tyne, UK
- Australia Plastic Surgery
- Westmead Hospital
- Royal North Shore Hospital
- Burns Unit, Concord Repatriation General Hospital
- Dr Jake Lim PLC
- AIDS and Cancer Virus Program, Frederick National Laboratory for Cancer Research, USA
- School of Health and Biomedical Sciences, RMIT University
- The Peter Doherty Institute for Infection and Immunity
- Emory Vaccine Centre, Atlanta, GA, USA
- Department of Dermatology, Royal Victoria Infirmary, Newcastle Hospital NHS Foundation Trust, Newcastle upon Tyne, UK