April 11, 2016 Print
Medical researchers from The Westmead Institute are investigating a new way to fight antibiotic-resistant bacterial “superbugs” by genetically manipulating the stubborn bacteria to be susceptible to drugs again.
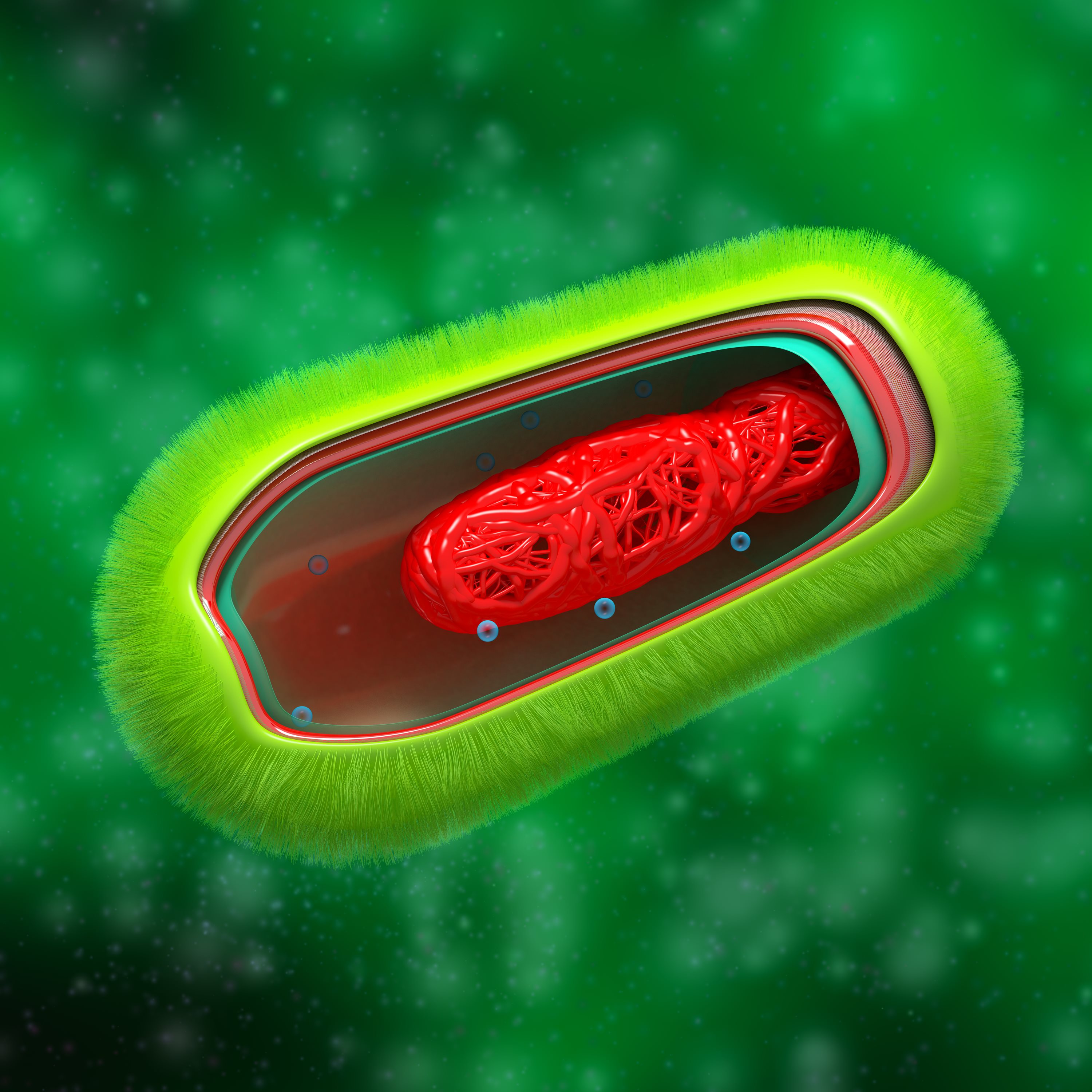 Bacteria - Prokaryote Cell Anatomy
Bacteria - Prokaryote Cell Anatomy
The promising technique could give hope to a global health system increasingly threatened by the growing inability of medicine to treat serious bacterial infections.
Some bacteria become resistant to an antibiotic through genetic mutations which produce potent chemicals that inactivate the drug. In other cases the bacteria eliminates the cell target that the antibiotic attacks.
Westmead Institute researchers are fighting back by using ‘therapeutic plasmids’ – specially constructed DNA molecules – to displace the antibiotic-resistant genes in the bacteria.
A plasmid is a type of genetic material in bacteria which replicates independently and can be transferred from host to host. This is bad news for humans when it comes to super strains of bacteria such as E. coli and Klebseilla, which are responsible for disease outbreaks around the world.
But the researchers - who are funded by the National Health and Medical Research Council - have turned this replication mechanism to their advantage by introducing a competitor plasmid onto the scene.
According to the Institute’s Critical Infection Group leader and Director of Infectious Diseases at the Westmead Hospital, Professor Jon Iredell, while the therapy is not a complete cure to antibiotic resistance, it is capable of ridding the real and emerging threat of antibiotic resistant gene-sharing gut bacteria.
This has been identified by the World Health Organisation as one of its top health priorities worldwide.
“Essentially, our therapy is a way of changing ‘bad’ (antibiotic resistant) bacteria into ‘good’ (antibiotic-sensitive) bacteria,” says Professor Iredell.
“Essentially, our therapy is a way of changing ‘bad’ (antibiotic resistant) bacteria into ‘good’ (antibiotic-sensitive) bacteria,” says Professor Iredell.
“We have already demonstrated in a mouse model that there is a way to manipulate these stubborn bacteria without killing them that allows them to become normally susceptible to antibiotics again, taking us back to where we were before antibiotic resistance became a problem.”
The researchers administered the therapeutic plasmids orally to the mice. Once ingested, these ‘good’ plasmids competed with the antibiotic resistant plasmids, leaving the mice with bacteria that were susceptible to antibiotics again. The Research Council grant will allow the team to extend this idea and develop applications in humans.
“We’ve shown that, just by feeding them a little bit of what is essentially the equivalent of yogurt, these bad plasmids are removed from the gut bacteria – gone permanently. It’s a system reset,” says Professor Iredell.
The next step for the researchers will be to replicate their findings in clinical trials but Professor Iredell says they are already part of the way there.
“We have already identified the types of problem plasmids that exist in people – we routinely look for these things. But at the moment, all we do is essentially isolate them and wait. If they develop into nasty infections our current approach is to enter the antibiotics arms race and cross our fingers."
Professor Iredell says the therapy is completely safe and removes the need for high-powered antibiotics.
“It doesn’t disrupt your ecosystem in the way that all of our other approaches do, and it doesn’t select for a whole bunch of new antibiotic resistance, which is the problem with the continuing escalation – the arms race – between antibiotics and bacteria.”
“There’s clearly an urgent need to identify strategies for dealing with antibiotic resistance, and this is the only positive approach to antibiotic resistance at the moment,” he says.
“There’s clearly an urgent need to identify strategies for dealing with antibiotic resistance, and this is the only positive approach to antibiotic resistance at the moment,” he says.